The coronavirus 2019 (COVID-19) epidemic spread throughout the world from the beginning of 2020, increasing healthcare professionals’ workloads and levels of physical and emotional stress.
AimsTo determine the prevalence of burnout syndrome in Spanish radiologists during the COVID-19 pandemic and the factors associated with the development of this syndrome, and to compare these findings with those obtained before the pandemic.
MethodsThis observation study took place between April 2020 and August 2020 (during the pandemic) through an online survey. A total of 150 responses were obtained. Demographic and work-related information was compiled. Burnout syndrome was measured with the Maslach Burnout Inventory Human Services Survey (MBI-HSS). The prevalence and characteristics of burnout syndrome obtained in this survey were compared with those of the same survey done in 2019. We performed a statistical analysis to identify possible risk factors and protective factors associated with this syndrome and to determine the homogeneity of the two samples.
ResultsThe prevalence of burnout syndrome increased during the COVID-19 pandemic (49.3% vs. 33.6%, p = 0.002). No risk factors or protective factors that were valid both before and after the pandemic were identified. No correlations were identified between sociodemographic or work-related characteristics and burnout syndrome.
ConclusionThis study demonstrates that burnout syndrome increased significantly in radiologists during the COVID-19 pandemic, affecting nearly half of all those who responded to the survey. These results underline the need to assess support for professional wellbeing of radiologists in Spain. No correlations were identified between burnout and gender, age, number of calls, years in the job, annual income, teaching, marital status, number of children, or type of contract.
La epidemia por coronavirus 2019 (COVID-19) se ha extendido por todo el mundo desde principios de 2020, sometiendo a los profesionales sanitarios a una sobrecarga laboral y a un mayor nivel de estrés físico y emocional.
ObjetivosEl objetivo de este estudio es determinar la prevalencia de desgaste profesional y sus posibles factores asociados en los radiólogos españoles durante la COVID-19, y su comparación con la situación previa a la pandemia.
MétodosEstudio observacional realizado entre los meses de abril y agosto de 2020 (durante la pandemia) mediante una encuesta en línea. Se obtuvieron un total de 150 respuestas. Se recopiló y comparó la información demográfica y laboral de los encuestados. Se determinó la presencia del desgaste profesional con el cuestionario Maslach Burnout Inventory Human Services Survey (MBI-HSS) y se comparó su prevalencia y características con el estudio realizado de la misma manera en 2019. Se hizo un análisis estadístico para identificar los posibles factores de riesgo y protectores asociados con este síndrome, así como un análisis de homogeneidad entre las dos muestras.
ResultadosLa prevalencia del síndrome aumentó de forma significativa (p = 0,002) durante la pandemia COVID-19 (49,3% frente a 33,6%). Ningún factor de riesgo o de protección se ha identificado como constante antes y después de la pandemia. No se he identificado ninguna correlación del desgaste con las características sociodemográficas o laborales.
ConclusiónEste estudio demuestra un aumento importante del desgaste profesional durante la pandemia por la COVID-19 con afectación de casi la mitad de los radiólogos encuestados. Estos resultados destacan la necesidad de valorar el apoyo orientado al bienestar profesional de los radiólogos en España. No se ha identificado correlación entre el síndrome y género, edad, número de guardias, antigüedad, ingreso anual, docencia, estado civil, número de hijos o tipo de contrato laboral.
Since the identification of the first patient infected with SARS-CoV-2 in December 2019 in Wuhan, China, and the declaration of the pandemic by the WHO on 11 March 2020, healthcare workers around the world have been subjected to highly stressful working conditions.1
Burnout is a psychological syndrome that develops as a negative reaction to work-related stressors, consisting of a combination of emotional exhaustion, depersonalisation and low personal accomplishment.2 Emotional exhaustion is related to an individual’s experience of stress, which, in turn, is related to diminished emotional and physical resources. Depersonalisation refers to detachment from work as a reaction to exhaustion overload and loss of enthusiasm and passion for carrying out work activities. Personal accomplishment refers to feelings of low professional efficacy and decreased work productivity.2
Concern for the well-being of workers has increased with the coronavirus disease (COVID-19), as they have had to work longer shifts associated with a greater emotional burden, which significantly affects the work-life balance.3 Limited healthcare resources and occupational risk associated with exposure to patients with this disease are conditions that affect the effective performance of professional practice.4
All these factors have contributed to the development of psychological disorders, with a significant increase in the prevalence of stress, exhaustion, insomnia, anxiety and depression.5 This situation has been identified in almost all medical specialities and has represented a challenge in terms of the exercising of professional activities during this pandemic.6
In Spain, all hospitals have adapted in a similar way to limit the exposure of its workers to COVID-19 and guarantee the proper functioning of the healthcare system, with variations depending on the prevalence of infection and government recommendations.7
Radiology is one of the specialities that had to be quickly reorganised because of the essential role it plays in screening, early diagnosis and assessment of the severity of COVID-19 lung involvement.8,9 Numerous articles have been published in the last year discussing the worrying increase in the prevalence of burnout among healthcare workers during the current COVID-19 pandemic. All this related mainly to workload, work-related stress and care pressure.3,10–13
The consequences of burnout are not limited to the health of the workers, but also affect the quality of care provided and organisational well-being.14,15 The prevalence of burnout syndrome had already increased in most Western countries even before the pandemic as a result of high levels of stress and the constant increase in workload.16–20 It may well be that the COVID-19 pandemic has exacerbated an existing problem within generally overburdened health systems, thus increasing the prevalence of this syndrome.11,12,19
This study analyses the characteristics and prevalence of burnout syndrome among radiologists in Spain during the COVID-19 pandemic and compares them with data obtained prior to the pandemic.
Material and methodsThis was a cross-sectional, observational, descriptive, analytical study carried out from April to August 2020, coinciding with a high peak of COVID-19 infections in Spain. Data were collected through the survey used previously,21 maintaining the same online, anonymous, voluntary method, using the Google® Forms application (Google LLC, Alphabet Inc., Mountain View, California, USA) and aimed at specialist radiologists and those in training who practice in Spain. At the beginning of the survey it was specified that participation was completely voluntary and that the data provided would be used completely anonymously and exclusively for research purposes. The study was approved by the Hospital Universitario y Politécnico la Fe Independent Ethics Committee in Valencia. The inclusion criterion applied was the completion of the Maslach Burnout Inventory - Human Services Survey (MBI-HSS). No responses were excluded. The direct link to the survey was shared on social media via email, WhatsApp, Twitter and Facebook. At the same time, the support and collaboration of the sections and subsidiaries of the Spanish radiological societies was requested in order to disseminate the link in their media outlets. There is no record of how many professionals and residents received this request.
The survey had three main sections (Appendix A, Annex 1). The first part was devoted to the MBI-HSS. This survey is endorsed in various studies carried out here in Spain. It is reliable and is considered valid for the assessment of burnout in multiple cultural and occupational settings.2,22 This MBI-HSS form includes three dimensions: emotional exhaustion with nine items, depersonalisation with five items, and personal accomplishment with eight items. Each of these 22 aspects is graded on a 7-point scale from 0 ("never") to 6 ("always"). These items are added together in each dimension to obtain a final score. Professional burnout was considered to exist when a score of 27 or above was obtained in the emotional exhaustion dimension, in addition to one of the following two scenarios: a score of 10 or above in depersonalisation and/or a score of 33 or below for personal accomplishment.23
The second section of the survey consisted of 13 questions about aspects associated with the sociodemographic, socioeconomic and work environment of the respondents (Annex 1). In the survey carried out during the pandemic, three questions were added on marital status, the number of children and the type of employment contract.
The third part included several questions focused on the radiologists' perception/opinion about possible causes of stress and factors that could improve their work situation (Annex 1).
From the database provided by Google® with all the responses to the survey, only subjects who completed the entire MBI-HSS were selected. The database had processes applied for data standardisation (both of the responses and their formats), regrouping of variables and levels (dichotomisation of the variables incentives, children and marital status; regrouping of autonomous communities into the Valencian Community, the Community of Madrid, Catalonia and others; assignment of numerical values to the ordinal categorical variables salary, shifts and years worked); and analysis of response coherence (detection of multiple answers in questions on the form with a single answer; compatibility of age with years of experience in radiology), followed by a descriptive analysis of the variables, both visual and numerical. Lastly, the processed database was used to perform different statistical analyses.
The influence of the different variables collected in the survey on the presence of burnout syndrome (Appendix A, Annex 2) was studied using the following statistical methods:
- •
To analyse the association of nominal categorical variables with the syndrome, the χ2 test of independence was used, as it is a hypothesis test referring to frequency distributions. With this method, if there is no dependence between the variables, it can be verified whether or not the observed frequencies in each category are compatible with the expected frequencies.
- □
The analysis of correlation of the different variables with burnout syndrome was performed by obtaining the following correlation coefficients: phi coefficient for dichotomous nominal categorical variables, Cramer's V coefficient for nominal categorical variables with more than two levels, Kendall’s tau coefficient for ordinal categorical variables, and point biserial r coefficient (based on Pearson's r coefficient) for quantitative variables.
- □
As this was a cross-sectional study, it was decided to perform the analysis of risk and protective factors against the syndrome by calculating the odds ratio (OR): an OR value greater than one will indicate a higher risk of suffering from the syndrome in those exposed to the factor, and vice versa. A value of 1 indicates that there is no relationship between the analysed factor and the syndrome. Therefore, when the 95% confidence interval (CI) for the OR includes this value (or when the p-value is greater than 0.05), the result is considered non-significant.
- □
The study was to be compared with the previously published study, carried out from January to July 2019.21 This comparator group is representative of the burnout syndrome in radiologists before the pandemic and allowed us to assess differences in the responses of radiologists in the two groups. The homogeneity analysis of the sociodemographic variables between the two samples (subjects who responded to the survey before the pandemic and during the pandemic) was performed using the χ2 goodness-of-fit test mentioned above in the case of categorical variables, and using the non-parametric Mann–Whitney U test for the quantitative variable of age. In the case of age, the Shapiro and D’Agostino normality tests24 were first carried out, choosing the non-parametric test to contrast the difference between the means because the results of these tests reflected a non-normal behaviour of the distribution of the age variable.
In all the statistical tests mentioned above, with the exception of the risk factor analysis, a p-value of less than 0.05 was established to consider the result significant. Both the database processing and the statistical analyses were performed using the Spyder (v4.1.4) and Jupyter Notebook (v6.0.3) software with Python version 3.8.3 and the Pandas (v1.0.5), NumPy (v1.18.5), SciPy (v1.5.0) and Statsmodels (v0.11.1) packages.
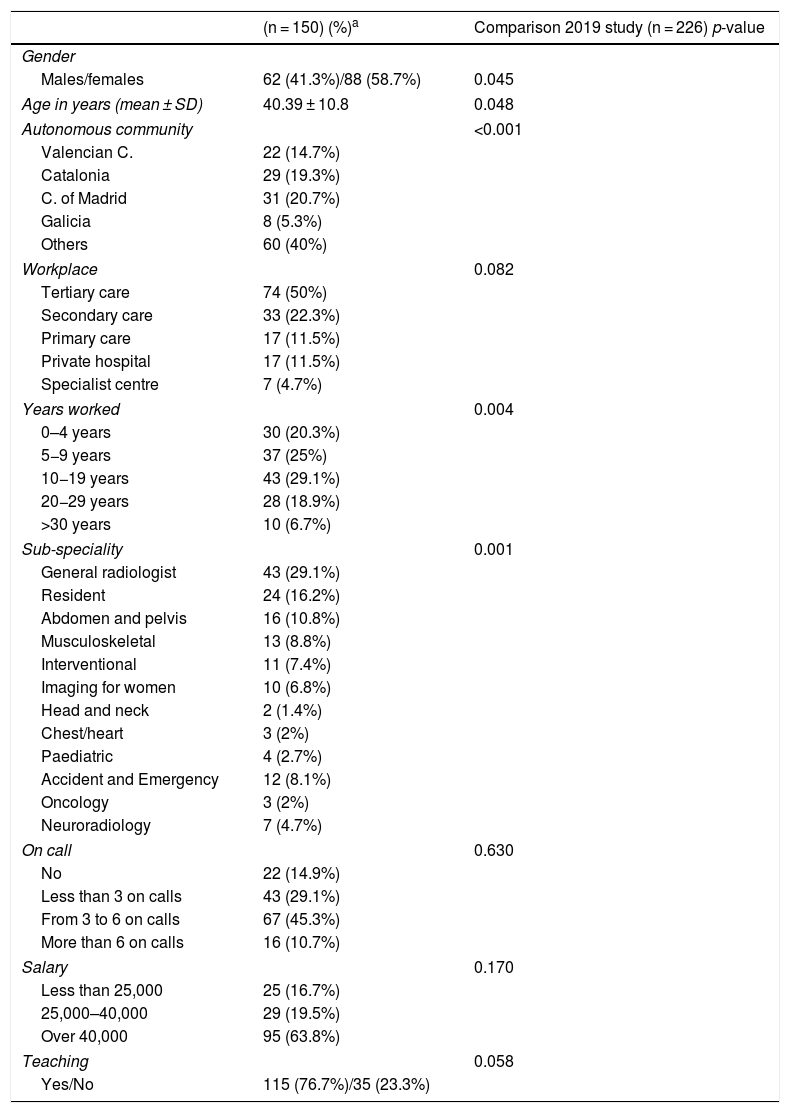
ResultsBetween April and August 2020 (during the COVID-19 pandemic), 150 radiologists completed the online form (Table 1). Of these, 20.7% were from the Community of Madrid (n = 31), 19.3% from Catalonia (n = 29), 14.7% from the Valencian Community (n = 22), and the remaining 45.3% from other autonomous communities (n = 68). In total, 58.7% (n = 88) of the respondents were female. The mean age was 40.4 ± 10.8 years, with a range of 23–70.
Sociodemographic characteristics of the sample.
| (n = 150) (%)a | Comparison 2019 study (n = 226) p-value | |
|---|---|---|
| Gender | ||
| Males/females | 62 (41.3%)/88 (58.7%) | 0.045 |
| Age in years (mean ± SD) | 40.39 ± 10.8 | 0.048 |
| Autonomous community | <0.001 | |
| Valencian C. | 22 (14.7%) | |
| Catalonia | 29 (19.3%) | |
| C. of Madrid | 31 (20.7%) | |
| Galicia | 8 (5.3%) | |
| Others | 60 (40%) | |
| Workplace | 0.082 | |
| Tertiary care | 74 (50%) | |
| Secondary care | 33 (22.3%) | |
| Primary care | 17 (11.5%) | |
| Private hospital | 17 (11.5%) | |
| Specialist centre | 7 (4.7%) | |
| Years worked | 0.004 | |
| 0–4 years | 30 (20.3%) | |
| 5−9 years | 37 (25%) | |
| 10−19 years | 43 (29.1%) | |
| 20−29 years | 28 (18.9%) | |
| >30 years | 10 (6.7%) | |
| Sub-speciality | 0.001 | |
| General radiologist | 43 (29.1%) | |
| Resident | 24 (16.2%) | |
| Abdomen and pelvis | 16 (10.8%) | |
| Musculoskeletal | 13 (8.8%) | |
| Interventional | 11 (7.4%) | |
| Imaging for women | 10 (6.8%) | |
| Head and neck | 2 (1.4%) | |
| Chest/heart | 3 (2%) | |
| Paediatric | 4 (2.7%) | |
| Accident and Emergency | 12 (8.1%) | |
| Oncology | 3 (2%) | |
| Neuroradiology | 7 (4.7%) | |
| On call | 0.630 | |
| No | 22 (14.9%) | |
| Less than 3 on calls | 43 (29.1%) | |
| From 3 to 6 on calls | 67 (45.3%) | |
| More than 6 on calls | 16 (10.7%) | |
| Salary | 0.170 | |
| Less than 25,000 | 25 (16.7%) | |
| 25,000–40,000 | 29 (19.5%) | |
| Over 40,000 | 95 (63.8%) | |
| Teaching | 0.058 | |
| Yes/No | 115 (76.7%)/35 (23.3%) | |
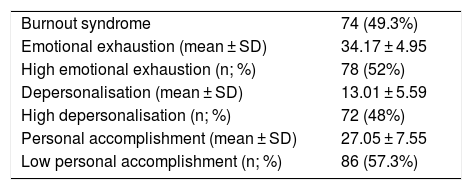
The prevalence of burnout syndrome during the pandemic (defined as high scores in emotional exhaustion and/or high in depersonalisation and/or low in personal accomplishment on the MBI-HSS) was 49.3% (n = 74) (Table 2). Broken down according to the survey's different dimensions, emotional exhaustion (a requirement for the diagnosis of burnout) was high in 52% (n = 78) of those surveyed. Depersonalisation was high in 48% of the respondents (n = 72) and low personal accomplishment was identified in 57.3% (n = 86).
Results of the dimensions that determine professional burnout among radiologists.
| Burnout syndrome | 74 (49.3%) |
| Emotional exhaustion (mean ± SD) | 34.17 ± 4.95 |
| High emotional exhaustion (n; %) | 78 (52%) |
| Depersonalisation (mean ± SD) | 13.01 ± 5.59 |
| High depersonalisation (n; %) | 72 (48%) |
| Personal accomplishment (mean ± SD) | 27.05 ± 7.55 |
| Low personal accomplishment (n; %) | 86 (57.3%) |
No risk factor for the development of burnout syndrome was identified in this study. In fact, working as radiologist of the abdomen and pelvis was identified as a protective factor (OR 0.2; 95% CI 0.06−0.75; p = 0.017). Although teaching in the workplace did not behave as a protective factor during the pandemic (OR 0.49, 95% CI 0.22–1.06; p = 0.06), it should be noted that the total prevalence of burnout among the respondents was 56.5% where no teaching was carried out versus 36.1% in centres with teaching.
No correlation was found between burnout syndrome and gender (0.04; p = 0.59), age (0.06; p = 0.47), number of on-call shifts (0.06; p = 0.42), years in post (0.03; p = 0.59), annual salary (0.09; p = 0.24), marital status (0.19; p = 0.19), children (0.04; p = 0.61) or type of employment contract (0.07; p = 0.96).
Table 1 shows the sociodemographic characteristics of the respondents during the COVID-19 pandemic. Comparing the prevalence of burnout syndrome among respondents during the pandemic and before the pandemic, there were significant differences (p = 0.002) between the two groups, with a prevalence of 49.3% during the pandemic and 33.6% in the pre-pandemic period.
With regard to the dimensions, there were no significant differences between depersonalisation (p = 0.22) and personal accomplishment (p = 0.73) during and before the pandemic.
The mean obtained from the respondents for emotional exhaustion during the pandemic was 34.17 ± 4.95, lower than the mean for the pre-pandemic sample (36.36 ± 5.6) (p = 0.012), but with a significantly higher prevalence of 52% (p = 0.008) (Table 2).
When analysing the possible improvements in mood between the groups of respondents with burnout syndrome, the only causes with significant differences between the two were reducing the number of shifts (75% pre-pandemic vs 57.4% pandemic; p = 0.028) and having an improvement in communication skills (53.4% pre-pandemic vs 69.6% pandemic; p = 0.048). No causes of stress with significant differences were found between the two groups.
Among the most common causes of improvement in mood, but without significant differences between the two groups with burnout syndrome, were: improvements in the organisation of the department (98.7% pre-pandemic vs 95.7% pandemic; p = 0.356); promoting teamwork (83.8% pre-pandemic vs 90.9% pandemic; p = 0.230); and increasing the number of people assigned to each of the activities (87.5% pre-pandemic vs 80% pandemic; p = 0.239).
Among the most common causes of stress in the two groups with burnout syndrome were: work being too chaotic, resulting in exhaustion (89.6% pre-pandemic vs 88.6% pandemic; p = 0.868); lack of control over work (87.3% pre-pandemic vs 76.8% pandemic; p = 0.113); and that the computer/program crashed easily (79.4% pre-pandemic vs 66.2% pandemic; p = 0.089).
DiscussionThis study identified that in radiologists who responded to the survey during the COVID-19 pandemic, the prevalence of burnout syndrome has increased significantly, from affecting a third of them prior to the pandemic,21 to half during the pandemic. Similarly, burnout syndrome among radiologists in the USA increased from 36% in 2013 to 46% in 2020.19,20 All of this points to an existing and prevalent problem among radiologists, which has most likely been exacerbated by the arrival of the pandemic. Other studies have identified a similar increase in the prevalence of burnout among healthcare workers since the COVID-19 pandemic began.3,12 Although in these studies the increase in emotional exhaustion and depersonalisation were correlated with the development of anxiety symptoms in women and depressive symptoms in men, we found no correlation with gender or any other sociodemographic or work-related data studied. We did not identify any risk or protective factors as significant and constant before and during the pandemic. Although working as radiologist of the abdomen and pelvis was identified as a protective factor in this study, we believe this result should be interpreted with caution and that more studies are needed to establish the true relationship with the presence of burnout syndrome.25 All this indicates that burnout among radiologists is a much more complex process than previously thought and that it cannot be associated with certain characteristics, as many are not causal and have a fluctuating relationship over time.
It may be that lack of motivation is related to an approach in radiology more focused on obtaining an imaging diagnosis than on the whole patient care process. For this very reason, the Working Group on Value-Based Imaging created by the European Society of Radiology has proposed a paradigm shift to emphasise the active role of the radiologist in day-to-day practice. This is intended to help the transition from volume-based to value-based healthcare. Value is defined as the health outcomes achieved for a patient (regardless of diagnosis) compared to the costs of achieving them.26
Since the appearance of the new coronavirus, an exponential and sudden increase in workload has been perceived, associated with uncertainty and the fear of becoming infected, leading to the perception of professional burnout and anxiety among all healthcare workers.1,4,27 In some parts of the world, because of the high incidence of COVID-19, health systems have almost collapsed under so much care pressure and have been forced to restructure and implement changes in their operations in a very short space of time.27,28 As COVID-19 mainly affects the respiratory system, causing characteristic patterns of pneumonia and thromboembolism, radiology departments were among those that had to adapt most quickly to this new situation.9,29,30 In this scenario of a catastrophic global pandemic, radiologists have had to learn very quickly to identify and assess the radiological manifestations of COVID-19, as, in the context of a severely oversaturated health system, clinicians have needed an orientative diagnosis in order to make treatment decisions.30 The high volume of requests for PCR plus the time necessary for adequate processing of the results have made imaging tests, particularly chest X-ray and tomography, essential for patient management; they help to grade the severity of the pulmonary or systemic involvement, and help in the assessment of prognosis and follow-up of these patients.9,30 All these changes have placed very heavy demands on radiologists, and chest radiologists in particular, as they have had to quickly adapt to new diagnostic challenges supported by little scientific evidence. In a study conducted in the USA, radiology is one of the specialist areas with the highest risk of developing burnout syndrome; it is classified as the speciality with the highest intellectual demand and comes third in time spent and effort required to reach a diagnosis.31 All these factors could explain the 16% increase in the prevalence of burnout syndrome in the group of radiologists who responded to this survey during the pandemic. Radiologists who were already vulnerable have become even more likely to suffer from burnout syndrome during the health crisis caused by COVID-19. This theory is supported by a decrease in the average score of those with high emotional exhaustion, and an increase in the prevalence of emotional exhaustion during the pandemic.
Both before and during the pandemic, in the final section of the survey, which aims to assess the respondents' subjective perception of the current situation facing radiologists in Spain in terms of burnout syndrome, of some concern is the high proportion of respondents who point to the need for improvements in the organisation of radiology departments in general, as well as increasing the number of radiologists and/or reducing the number of studies assigned to each one. In line with our study, in the survey carried out in Europe by the European Society of Radiology (ESR), almost half of the radiologists referred to the need to reduce the daily workload.32
This study shows that the perception of radiologists in Spain about the possible causes of work-related stress has not changed with the appearance of the pandemic, pointing to the need for improvements in organisation and IT resources. Chetlen et al. reported prior to the pandemic that burnout syndrome in radiology was correlated with increased workload, occupational stress and little time allocated for studies, poor organisational support and limited computing resources.19 With regard to workload, burnout syndrome among radiologists worldwide was assessed and brought to the fore by several articles published prior to the pandemic, most of which related burnout to the computer boom, the increase in imaging tests performed, the large number of images that have to be examined per patient, the introduction of electronic records, long working hours, conflicting time demands (clinical, academic, administrative), insufficient staff to complete the routine tasks and the inability to reconcile personal and professional life.15,18,33–35
One of the main sources of stress reported by the majority of those surveyed, both before and during COVID-19, is program or computer failure, slowing down the performance of routine tasks and creating the sensation of lack of control over their work.15,18,19 Excessive working with screens without adequate breaks can trigger visual fatigue in radiologists, which can affect diagnostic accuracy.36 This can give rise to diagnostic errors, with the fear and responsibility that this entails increasing emotional exhaustion, leading to professional burnout.15
Although no relationship has been identified between being on call and burnout syndrome, it is comprehensible that more than half of those surveyed before and during the pandemic point to being on call as a source of stress. The fact that excessive working hours and circadian rhythm disorders negatively affect doctors is widely described and documented in the specialised literature.14
It is striking that in the group with burnout syndrome, there is a very high perception of the work environment as "chaotic and exhausting", with this not meeting the workers’ expectations and even leading to feelings of "boredom or disinterest" and a desire to change career path. Over time, all this can translate into increased emotional exhaustion and depersonalisation on the part of the radiologist.19
Among the possible improvements most mentioned by the survey respondents are those related to the workplace. The majority of those surveyed before and during the pandemic indicated that they wanted to improve their communication skills, foster teamwork and even establish friendships with colleagues outside of the work environment. These possibilities may represent viable strategies that could be applied by radiology departments.37,38
Interestingly, a significant increase in the desire to improve communication skills was identified among those surveyed during the pandemic. If the nature of the radiologist's work was already solitary, with the arrival of the pandemic and the need to maintain safe distancing, structural changes were made in departments which reduced human interaction, further increasing radiologists' feelings of isolation. An improvement in communication skills could therefore help alleviate the stress caused by insufficient time, which rarely allows adequate communication with colleagues, other specialists or the patient.32 In a survey carried out by the ESR, 75% of the radiologists stated that they were frequently in contact with other specialists or patients and, of these, over 70% felt they did not have enough time for adequate communication.32
Now this situation has been identified, it is essential to recognise the factors affecting the well-being and resilience of radiologists, in order to initiate organisational and individual interventions for the management and reduction of burnout syndrome.39
This study has several limitations. Although the response rate was relatively low in relation to the estimated total population of radiologists in Spain (6000 members of the Spanish Society of Medical Radiology [SERAM]), the sample is considered representative of the situation in Spanish radiology. We believe that the prevalence identified in this study can be considered to be the proportion of radiologists who suffer from burnout syndrome with respect to the total population evaluated. However, the problem of representativeness was minimised, as there was no bias in the selection of radiologists who received the survey. With the radiology residency program offering 260 places per year with a duration of four years, the total number of residents represents approximately 17% of radiologists, a very similar proportion to that obtained in this sample (16.2%). Although there are differences between gender, autonomous community, age, years worked and speciality, we believe these differences are small, indicate greater representativeness of the sample and do not bias the specific comparison made. The percentage of women who participated in both surveys was similar to the proportion of female radiologists (53.8% in 2018).40 The distribution by autonomous community in Spain is not balanced, but we believe the health system is reasonably similar from one autonomous community to another in aspects relating to burnout syndrome. As this was a voluntary survey, there is likely to have been a self-selection bias, as radiologists close to burnout syndrome were probably more likely to respond to the survey and complete it with more care and attention than those not suffering from burnout. In contrast, if they were over-stressed as a result of the pandemic, they may not have been interested in responding to the survey. At the same time, as the survey was anonymous, we cannot rule out there being people who responded to it more than once. Personality traits or psychological characteristics of each individual were not considered among the possible predictors of burnout syndrome.
Other contextual and organisational variables that might have played a significant role in predicting burnout may not have been included in the analysis.
ConclusionIn this study, we found an increase in the prevalence of professional burnout among radiologists in Spain during the COVID-19 pandemic, with almost half of respondents being affected compared to a third of surveyed radiologists prior to the pandemic.
We believe that these results may be explained by exacerbation of problems that already existed prior to the pandemic, which, combined with the health crisis caused by COVID-19, have affected radiologists who are vulnerable to or at risk of suffering from this syndrome.
Authorship- 1
Responsible for the integrity of the study: AO and EBA.
- 2
Conception of the article: AO, EBA, CBD and LMB.
- 3
Design of the article: AO, EBA, CBD and LMB.
- 4
Data collection: AO, EBA and LMB.
- 5
Data analysis and interpretation: AO, EBA, CBD and LMB.
- 6
Statistical processing: AO, EBA, CBD and LMB.
- 7
Literature search: AO, EBA and LMB.
- 8
Drafting of the article: AO, EBA, CBD and LMB.
- 9
Critical review of the manuscript with intellectually relevant contributions: AO, EBA, CBD and LMB.
- 10
Approval of the final version: AO, EBA, CBD and LMB.
This study received no specific grants from public agencies, the commercial sector or non-profit organisations.
Conflict of interestThe authors declare that they have no conflicts of interest.
The authors would like to thank all the participating radiologists for their selfless participation and collaboration.
Please cite this article as: Oprisan A, Baettig-Arriagada E, Baeza-Delgado C, Martí-Bonmatí L. Prevalencia y factores de desgaste profesional en radiólogos durante la pandemia COVID-19. Radiología. 2022;64:119–127.